-
Franks A, Curtis C, Barker S. Velamentous Cord: A Dangerous Case Complicated by a Rural Population. Marshall Journal of Medicine. 2015;1(1): Article 8. DOI: 10.18590/mjm.2015.vol1.iss1.8.
-
Franks AM, Guzzo R, Barker S, King-Mallory R. Progressive Supranuclear Palsy – A Case Study from the Perspective of a Primary Care Physician Son. WVMJ. Jan/Feb 2017; 113(1):36-9. PMID: 29373002
-
Franks AM, Fischer R, Plummer A, Nettey R. Poland Syndrome: A Case of a Left Handed Infant. WVMJ-OA. April 2017; DOI: 10.21885/wvmj.2017.8.
-
Franks A, Petrany SM, McElroy S, Alley A. The Marshall Family Medicine Residency twINTERN Schedule: The Impact of an Innovative Hospital Coverage Scheme on Resident Fatigue. Fam Med. June 2017;49(6):468-472. PMID: 28633175
-
McCann KS, Barker S, Cousins R, Franks A, McDaniel C, Petrany S, Riley E. Structures Management of Chronic Nonmalignant Pain with Opioids in a Rural Primary Care Office. JABFM. Jan/Feb 2018;31(1):57-63. DOI: 10.3122/jabfm.2018.01.170163. PMID: 29330240
-
Jarrell A, Mays A, Bannister T, Franks A. Cobalamin Deficient Thrombotic Microangiopathy: a Case of TTP or Pseudo-TTP. WVMJ-OA. April 2018; DOI: 10.21885/wvmj.2018.5.
-
Franks A, McCann K, Saab M, Bell K. Chronic Fatigue Syndrome Through Postural Orthostatic Tachycardia Syndrome to Hypermobile Ehlers Danlos Syndrome: a Journey Through Unclear Diagnoses. WVMJ-OA. June 2018; DOI: 10.21885/wvmj.2018.8.
-
Franks AM, Urian JW, Patton R, Barker S. A Shocking Etiology of Placental Abruption: a Case of Electric Shock During Pregnancy. WVMJ-OA. July/August 2018;114(4):26-29.
-
King-Mallory R, Barker S, McGrogan K, Franks A. Nadolol in Pregnancy: A medical student’s reflection on her pregnancy. Marshall Journal of Medicine. 2018;4(4): Article 5. DOI: 10.18590/mjm.2018.vol4.iss4.5.
-
Krauss A, Barker S, Franks, A. Revisiting Peripartum Cardiomyopathy: A Subsequent Pregnancy. WVMJ-OA. Nov 2018; DOI: 10.21885/wvmj.2018.16.
-
Seaman C, Amos M, Franks A, Sexton A, McClelland K, Harris E. Diabetic Muscle Infarction: A Rare End-Organ Vascular Complication of Diabetes. MJM 5(4)28-37.
-
Rodriguez K, Wellman C, Franks A, McClelland K, Bannister T. Pigmentary and Other Dermatologic Manifestations of Minocycline: a reminder of adverse effects. MJM 5(4)21-7.
-
Pellegrini VD Jr, Franks AM, Englander R. Finding Greater Value in the Fourth Year of Medical School: Accelerating the Transition to Residency. Acad Med. 2020 Apr;95(4):527-533. doi: 10.1097/ACM.0000000000003049. PMID: 31651433
-
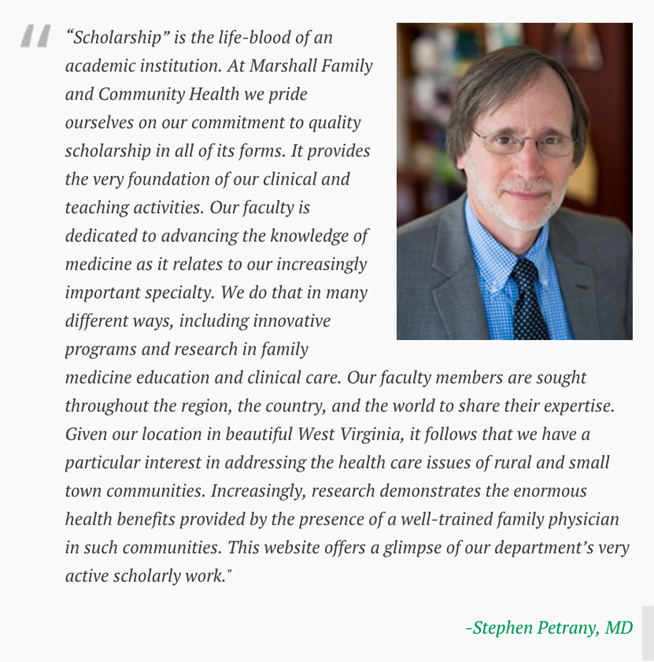
Franks AM, Petrany SM. Building a Culture of Scholarship Within a Family Medicine Department: a Successful Eight-Year Journey of Incremental Interventions Following a Historical Perspective of Family Medicine ResearchMedical Science Educator, (), DOI: 10.1007/s40670-020-01107-81-6
-
Dever J, Franks AM, Given LM, Rollyson W, Mays-Kingston A. Chronic Inflammatory Demyelinating Polyneuropathy (CIDP) in a Patient with Diabetes: a primary care perspective. MJM 6(4). DOI: 10.33470/2379-9536.1277
-
Rupp DP, Huth C, Stickler K, Franks A, Rollyson W, Freeman WT, Giangarra C, Ours D. Shoulder Pain in a Weight-Lifting Adolescent Athlete: A Zoonotic Etiology. Cur Sports Med Rep Dec 2020: 19(12):517-21.
-
Lester, Paige MS II; Franks, Adam M. MD; Rollyson, William MS IV; Barbour, Jenna K. MD; and Curry, Matthew B. MD (2021) "Anti-N-Methyl-D-Aspartate Receptor Encephalitis: a diagnosis obscured by concomitant recreational drug use," Marshall Journal of Medicine: Vol. 7: Iss. 3, Article 5. DOI: 10.33470/2379-9536.1281
-
Wendt BJ, Franks AM, Dusing SLO, Hess KL, O’Hanlon, KM, Petrany, SM. Penile Variant of Mondor’s Disease: A Challenging Diagnosis Requiring Primary Care and Urologic Collaboration. WVMJ-OA. June 2021; 40-3.
-
Franks, AM, Murphy M, Griffis M, Franks R, Franks CM, Petty G. “Alpha Gal Allergy: a new threat to Appalachia.” Marshall Journal of Medicine: Vol. 7: Iss. 4, Article 2. DOI: 10.33470/2379-9536.1348
-
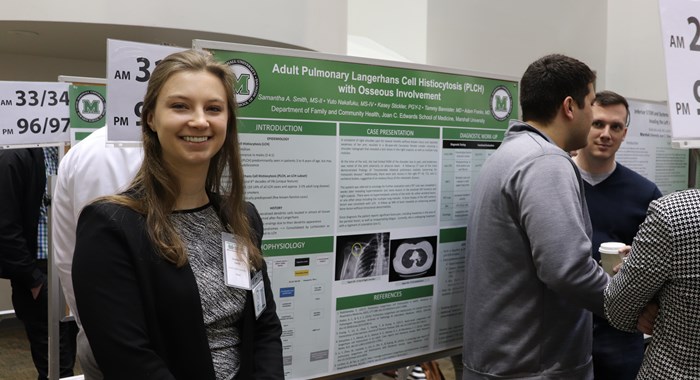
Smith, Samantha A. MS III; Franks, Adam M. MD; Rollyson, William MS IV; Griswold, Doreen; and Bannister, Tammy MD. "Adult Pulmonary Langerhans Cell Histiocytosis with Osseous Involvement: understanding this rare mimic of malignancy," Marshall Journal of Medicine: Vol. 8: Iss. 1, Article 4. DOI: 10.33470/2379-9536 HYPERLINK "https://doi.org/10.33470/2379-9536.1276".1276
-
Wellman, Courtney MD; Ratcliffe, Jordan BS; Rollyson, William MD; Franks, Adam M. MD; Grome, Mike PA-C; and Walker, Robert MD. "Over-the-Counter Analgesic Use Patterns in Appalachian Older Adults, Focusing on Non-Steroidal Anti-Inflammatory Drugs," Marshall Journal of Medicine: Vol. 8: Iss. 1, Article 5. DOI: 10.33470/2379-9536.1336
-
Chongswatdi, Natavoot N. MD; Seaman, Callie MD; Harman, Diane RN, BSN; Rollyson, William MD; and Franks, Adam M. MD (2022) "Analysis of Blood Borne Pathogen Exposure Monitoring Protocol Adherence in an Academic Medical Center: a seven year analysis and literature review," Marshall Journal of Medicine: Vol. 8: Iss. 2, Article 6. DOI: 10.33470/2379-9536.1358
-
Franks Adam M MD, Calamur Nandini MD, Dobrian Anca PhD, Danielson Mark PhD, Neumann Serina E PhD, Cowan Eileen MD, Weiler Tracy. Rank and Tenure Amongst Faculty at Academic Medical Centers: A Study of More than 50 Years of Gender Disparities. Acad Med
-
Franks, Adam M MD, McCann, Kevin S MD, Velthouse, Kimberly MD, Sutphin, Rich MPH, Davies, Todd PHD, Petrany, Stephen M MD. Intentional Structured Opioid Monitoring Protocol: Responsible and Viable Deprescribing – Accepted WVMJ
-
Franks, Adam M MD, Seaman, Callie MD, Franks, Emily MA, CCC-SLP, Rollyson, William MD, Davies, Todd PhD. Reading at Least One Book a Day to Children Less Than 1 Year Old: an analysis of language score impact and parental motivation strategies in a family medicine practice. - Accepted JABFM